February 26, 2024 02:24 PM

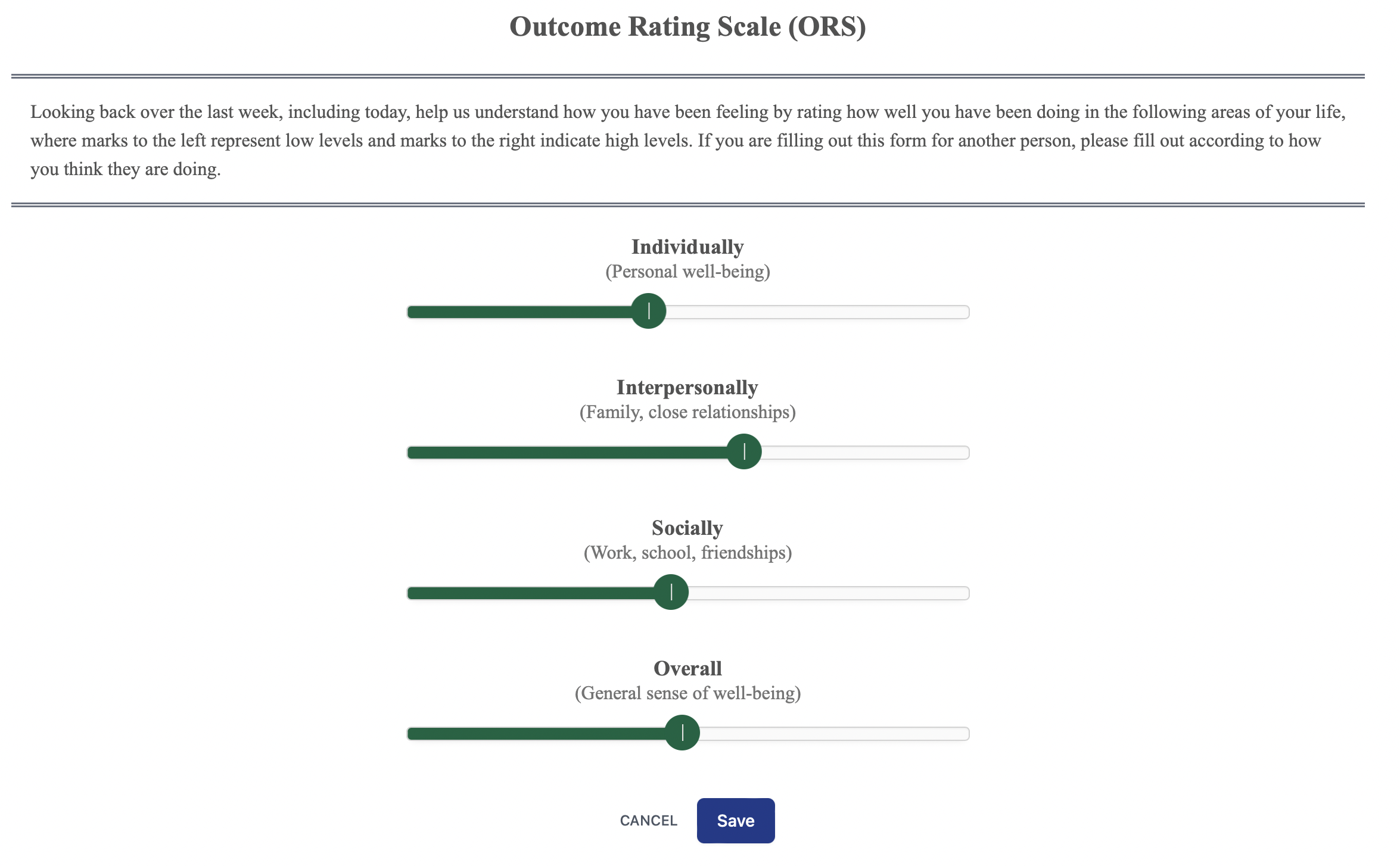
The Outcome Rating Scale (ORS) is the first of two brief, user-friendly measures employed by the Partners for Change Outcome Management System (PCOMS). The ORS measures client benefit from services while the Session Rating Scale (SRS) solicits client views about the therapeutic alliance. The ORS, however, is far more than simply a measure of benefit. There are three functions or faces of the Outcome Rating Scale: 1. A collaborative, communicative process designed to privilege clients, involve them in decision-making as true partners, and tailor services to their resources and needs; 2. A normative, psychometrically sound measure of outcome with studies supporting its reliability, validity, and metrics of change (reliable and clinically significant change), as well as algorithms for expected treatment response (ETR); and 3. A method to operationalize a multicultural orientation, to explore and validate the client’s experience of marginalization and discrimination.
Outcome Rating Scale (ORS): Collaborative and Communicative
PCOMS represents a departure from expert-driven formulations that attempt to classify client distress and problems of living from a theoretical or symptom vantage point. Instead, clients are empowered to highlight their views of distress/well-being, refocusing therapy toward individualized problem construction and collaborative solution building and away from options based on diagnosis, symptomology, or normative functioning. Unlike other validated outcome instruments, the ORS is not a list of symptoms or problems checked by clients on a Likert scale; it is not forced choice or symptom-oriented. Rather it is an instrument that is individualized with each client to represent their idiosyncratic experience and reasons for service. A hallmark of the ORS and PCOMS is that it involves clients in all decisions that affect care. ORS scores are discussed and client viewpoints are solicited in each session.
Outcome Rating Scale (ORS): Normative and Psychometrically Sound
Despite its brevity, multiple validation studies of the ORS as well as efficacy studies have found that the ORS generates reliable scores. Coefficient alphas have ranged from .87 to .91 in validation studies and from .83 to .92 in clinical studies. Research also suggests that the ORS generates valid scores as a measure of general distress. Three studies found evidence of concurrent validity for the ORS by comparing ORS scores to the OQ as well as with symptom and diagnosis-based measures, like the Symptom Checklist-90–Revised and the Patient Health Questionnaire 9
BON displays a client’s status in relation to the expected treatment response (ETR) and normatively determined clinical cutoffs (25, ORS for adults). The client’s initial total ORS score generates an ETR line based on algorithms derived from extensive administrations of the instrument. The ETR in BON serves as a trail map via a progress meter that reports the percent of the ETR achieved at each session, alerting the client and clinician when to become concerned. At a minimum, this information helps clinicians and supervisors prioritize their efforts and plan for remedial treatment strategies. More importantly, red flags call attention to the need to immediately discuss new directions with clients.
Outcome Rating Scale (ORS): Cultural Responsiveness
Beyond ensuring representative diversity and educating dominant culture practitioners about privilege and other biases, less has been proposed about doing culturally responsive work with this client with this therapist. PCOMS provides an example of how any feedback system can address client experiences of marginalization and discrimination as well as differences between client and therapist. The content-free dimensions of the PCOMS measures allow clients to describe the meaning of their scores without preconceived theoretical or symptom-based constraints. Thus, client accounts retain the richness of real life, including the unique backstories that contextualize their dilemmas. In relating their stories, clients color in the even more specific details of their unique life situations.
Conversations generated by client scores on the ORS are openings for therapists to inquire about clients’ reasons for service, views on precipitating and contextual factors, the impact of the problem in clients’ lives, and thoughts about general directions for problem resolution. The ORS contextualizes presenting problems beyond diagnostic categories, running counter to practices that pathologize clients of color and other historically marginalized groups at higher rates. Putting client reasons for service in context also promotes consciousness-raising for both client and therapist, helping to identify forms of oppression and marginalization that may contribute to distress. Consequently, the Outcome Rating Scale creates opportunities for cultural awareness and responsiveness. It provides a logical place for such conversations to occur if they do not do so naturally during treatment, enabling the space to make humble attempts at getting closer to the client’s unique experience.
Cultural competence takes a sustained effort to include clients and embrace their feedback—to not reduce psychotherapy to the medical model equation of diagnosis plus prescriptive treatment equals cure, nor clients to cultural, ethnic, racial, or gender stereotypes or pharmaceutical-sponsored checklists, nor the proclivities of enlightened psychotherapists who know better than clients what they need. The ORS helps this effort.
Unlocking Multicultural Competence: How Systematic Client Feedback Transforms Psychotherapy Practice
An article addressing this face of the ORS and PCOMS is coming soon in the journal, Psychotherapy. Here is the abstract:
There have been great strides in psychology regarding diversity, equity, inclusion, and multicultural competence, but a need remains to translate these values into actionable practices in psychotherapy. While the case has been made that measurement-based care is an evidenced-based intervention that improves outcomes and reduces dropouts (de Jong et al., 2021), and recently, that it provides a transparent collaborative process to engage clients in treatment (Boswell et al., 2023), it has not been widely considered as a methodology for multicultural competence. We trace the evolution of what was once called “patient-focused research” (Lambert, 2001) and identify a significant change in recent writings to include important clinical and collaborative processes, a transition from a strictly normative or nomothetic understanding of the value of feedback to an appreciation of its communicative or idiographic processes. We propose that systematic client feedback promotes a “multicultural orientation” (Owen, 2013) at the individual therapist-client level, that client responses to outcome and process measures can foster cultural humility and create cultural opportunities (Hook et al., 2017) to address marginalization and other sociocultural factors relevant to treatment. Using one system to illustrate what is possible for all feedback approaches, we present client examples that demonstrate an integration of a multicultural orientation. We suggest that systematic client feedback can provide a structure to address diversity, marginalization, and privilege in psychotherapy.
Email Barry at barrylduncan@comcast.net for a pre-pub copy.





.png)


.png)