June 04, 2019 09:36 AM

Two randomized clinical trials confirm that the Partners for Change Outcome Management System (PCOMS) improves outcomes and reduces dropouts in group therapy with both mental health and substance abuse problems, and with voluntary and mandated consumers.
Using PCOMS in groups naturally amplifies client voice and provides a fertile place to increase participants’ appreciation of their own and others’ perspectives. A great thing about group therapy is that discussions with clients about ideas for getting on track, or back on track, can be further supported by contributions from group participants.
Nuts and Bolts
- Who and How Often: Depending on the setting (inpatient, residential, intensive outpatient, etc.), clients may receive several services delivered by different providers over various periods of time. Consequently, PCOMS implementation requires a decision about which service makes the most sense to administer the measures, who will do it, and at what frequency. Once-a-week administration of the Outcome Rating Scale (ORS) combined with the administration of the Session Rating Scale (SRS) or Group SRS for each service provided is the general rule. An exception here is if length of stay is 10 days or less (e.g., acute inpatient programs), which will require more frequent administration. PCOMS can be successfully implemented in either individual or group therapy services as long as there is adequate time for review and discussion of the client scores. If the decision is to administer the ORS in individual services, which often makes the most sense, the Group SRS should be administered in group therapy.
- Group Admin Logistics: ORS and Group SRS administration vary depending on how often and how long the group meets. Reviewing both the ORS and Group SRS in one group therapy session can be challenging depending on session length and how much content must be covered. In residential, inpatient, and intensive outpatient settings with longer groups (2½ or 3 hours), both scales can be administered within the same group. However, if you are doing 2-hour or fewer groups that meet only once a week, alternate the focus each week (i.e., do the ORS one week and then the Group SRS during the next group session). If your group meets more than one time per week, administer the ORS at the beginning of the first meeting and the Group SRS at the beginning of the last meeting of the week. This allows you to successfully integrate PCOMS in a manageable way while still attending to the purpose of the group. PCOMS is not intended to replace group content, but rather to efficiently monitor the group’s effects on client benefit and the experience of the group process.
- Responsibility and Graphing: Using PCOMS with groups requires that participants take responsibility for PCOMS as part of the group culture. The group leader or facilitator starts this process during a pre-group individual session or an orientation group by teaching the use of Better Outcomes Now (BON), or if using the paper and pencil measures, the Self-Completed Overview of Resilience Experience (SCORE) Board. PCOMS in groups works best when clients come in a few minutes early, complete the ORS (or Group SRS), and graph their scores. As a web application, BON has the advantage of automatically displaying graphed results after the client takes the ORS/Group SRS. Group members can also take the ORS at home before they come to group therapy using BON’s remote functionality. Graphing is essential. Graphs help participants visualize change while tracking progress on goals:
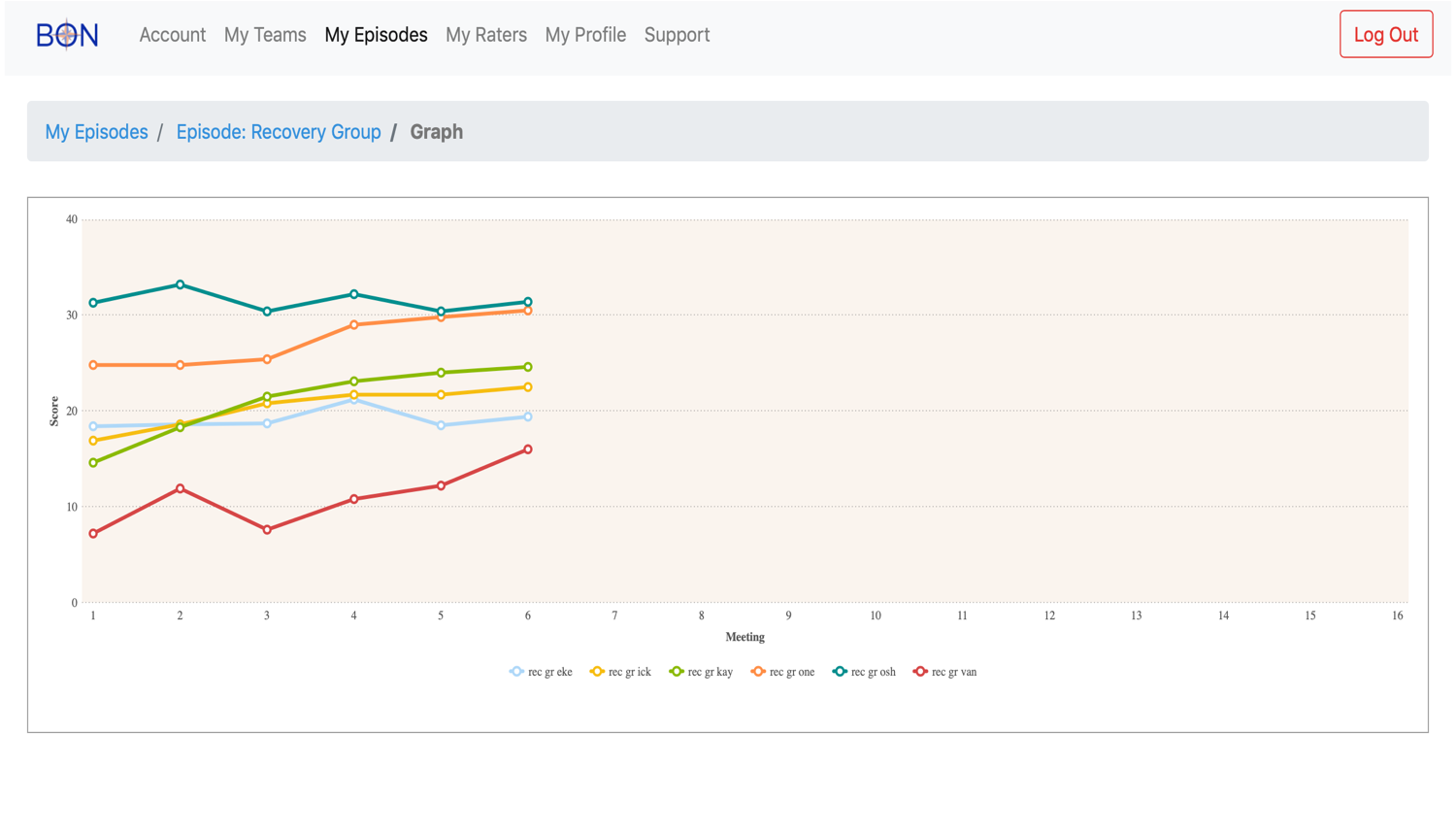
- Discussion: Discussing each participant’s ORS scores may take 15-30 minutes depending on the size of the group. Start with “Whose scores went up? What did you do or experience that was different from previous weeks?” Then prompt supportive feedback from others so that the participant feels heard, understood, and respected. Hone in on the changes, validate and celebrate them, and ensure clients take ownership of what they did to make the changes happen. Follow that by asking, “Whose scores didn’t change?” and validate those reported experiences. Then, use the group process to have the more successful folks say what is working for them as well as soliciting suggestions from the group in total. BON provides the group leader with a graph that displays all the group member scores for ready reference to who is benefiting and who is not.
Read more about PCOMS and group therapy in George Braucht’s chapter in the new PCOMS manual, and request a free trial of BON now:





.png)


.png)