February 16, 2022 11:13 AM
The Outcome Rating Scale (ORS), the measure of the Partners for Change Outcome Management System (ORS), is quite different than other outcome instruments. It is an outcome measure, but it is also a valuable clinical tool that requires nuance in its use. It is not a perfunctory piece of paper to be flicked at clients to tick off a box or satisfy a management edict. It is an evidence-based practice to improve client care.
To make proper use of twenty years of psychometric validation and thirteen years of research demonstrating dramatically better outcomes and reduced dropouts, the ORS requires four steps. Barry Duncan, the developer of the clinical process of PCOMS, identified four essential components of doing the evidence-based practice, the Partners for Change Outcome Management System (PCOMS) to fidelity. The previous blog covered the first two. This blog covers the last two steps, including the most important clinical nuance of using the ORS.

Skill Three: Connect the client’s marks/touches on the ORS to the described reasons for service. Ensure that the ORS is not used as an “emotional thermometer” or an account of how life is going. Refer to the ORS during the encounter.
This is the most important clinical nuance of PCOMS. The ORS and SRS are not like bread to a sandwich, separate from the real meat of the session. Rather, they are clinical tools intimately integrated into the work itself. The ORS is not an emotional thermometer that rates how the client is feeling at the moment it is given nor is it intended to be an ongoing account of how the client’s life is going week to week. Rather, the ORS is designed to measure how things are going in the client’s life relative to the reasons for service.
The ORS, by design, is a general outcome instrument and provides no specific content other than the broad domains. It offers a bare skeleton to which clients must add the flesh and blood of their experiences, into which they breathe life with their perceptions. At the moment in which clients connect the marks on the ORS with the situations that are distressing, and to what they would like to accomplish, the ORS becomes a meaningful measure of their progress and a potent clinical tool.
Because the ORS has face validity, clients usually mark the scale the lowest that represents the reason they are seeking services and often connect that reason to the mark they’ve made. Although some will refer to their touches on the ORS, with other clients, you may need to clarify the connection between the client’s descriptions of the reasons for service and the client’s marks on the ORS. This entails eliciting the client’s perspective on what the marks mean so that you are on the “same page” regarding what the marks say about the work and whether the client is making any gains. This way, both you and the client know what the mark on the line represents to the client and what will need to happen so that the client will both realize a change and indicate that change on the ORS.
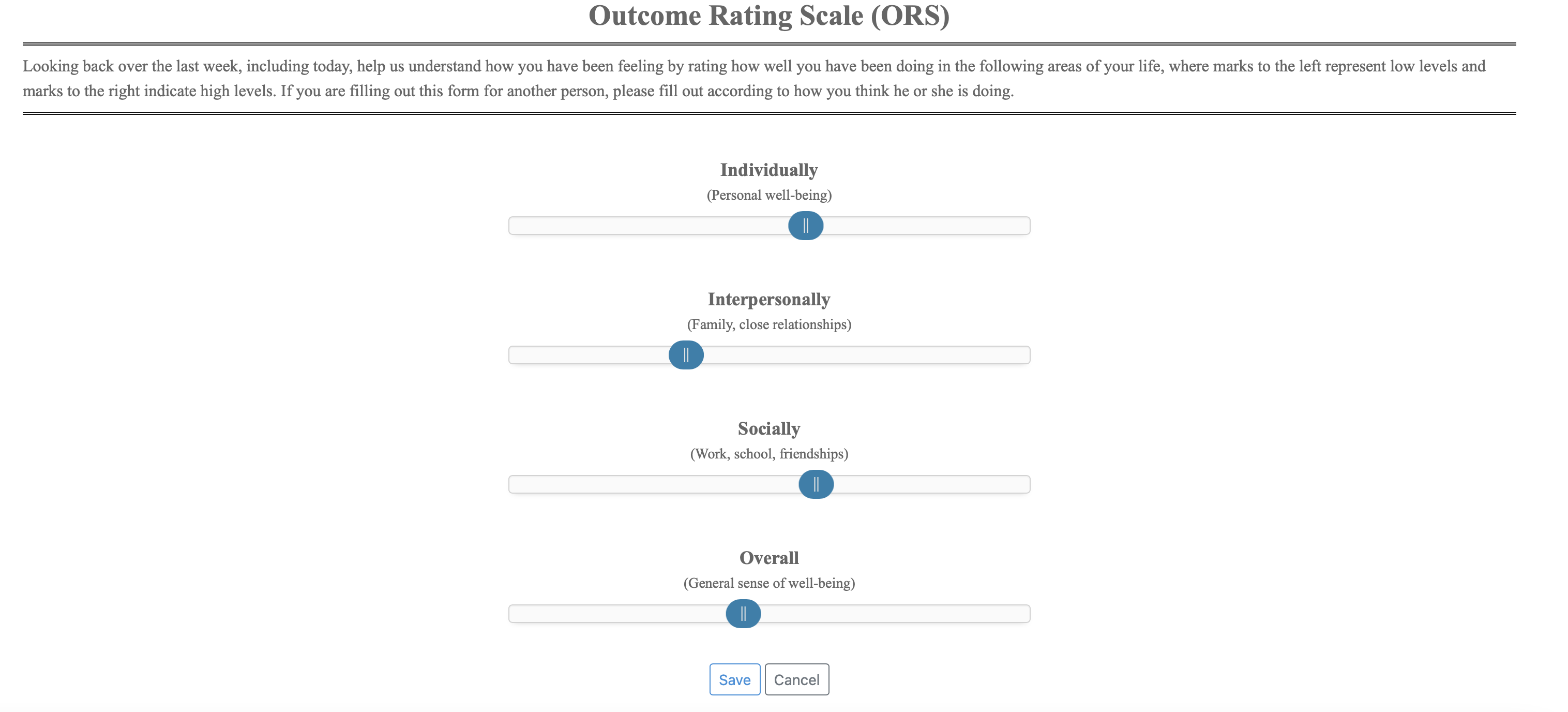
At some point in the meeting, the provider needs only to pick up on the client’s comments and connect them to the ORS:
Okay, it sounds like dealing with the loss of your job (or relationship with partner, sister’s drinking, or anxiety attacks, etc.) is an important part of what we are doing here. Does the distress from that situation account for your mark here on the blank scale on the ORS? Okay, so what do you think will need to happen for that mark to move just one centimeter to the right?
It is important that the client understands that the marks on the scales should be connected to and reflect those issues that are the grist for the mill. From the get-go, ensure that the measure is relevant to both the client’s experience and the work that will ensue. If that connection isn’t made, then the ORS becomes an emotional thermometer reading of weekly moods in response to the inevitable ups and downs of life. And then it is worthless.
Most of the time, there will be one scale lower than the rest, one that reflects the greatest distress. You can note the lowest scale at the start of the conversation when you invite the client to start with that scale or wherever they would like. Then as the client discusses the issue that is represented by that distress, explicitly connect that mark or touch on that line with the client’s description of the distress. Follow this with questions about what it would take to move the mark just 1 cm to the right.
When all scales are low, and after the client describes the distress in their life, ask the client where they will likely see the gain first if your work with them is successful. Then proceed with goal and theory of change questions.
Finally, connecting the client’s experience to the ORS has other benefits. It can help you and the client stay on track by providing a way to focus the session back on the lowest-rated scale when the conversation goes astray—the ORS helps prioritize topics as well as thematically tie different elements of the discussion together. Simply pick up your device displaying the graph page and ORS, and redirect to the issue at hand as well as what can be done in the session and beyond to move the mark to the right.
Skill Four: Get an accurate rating of the ORS; i.e., a rating that matches the client’s description of their life circumstance and reasons for service. Immediately clarify mismatches and redo the ORS.
Given that the first ORS provides the comparison point for all future work with the client, it is essential to get a good rating. This means striving to get the most accurate rating of the client’s experience possible, a sincere appraisal of their life. Encourage a frank discussion of the issues involved, express your desire to be helpful, and get the idea across that therapy works best when the ORS is an accurate reflection. In general, any score above 32 is not a good rating, certainly one to be cognizant of whether it matches the client’s description of their life. Even people who consider themselves doing very well in life do not tend to rate this high.
There are three reasons that people score above 32 on a first meeting ORS:
- Either they don’t understand the ORS;
- They are disgruntled and are blowing it off;
- Or they are frightened about the consequences of showing any distress.
None of these reasons is difficult to overcome with transparent conversation.
Clients who rate the ORS over 32 and then after a few minutes start telling you how bad their life is going do not understand the measure. All you have to do is ask about it and perhaps the easiest way is to simply inquire where the distress that the client is describing can be found on the ORS. Transparency is the rule. Just ask clients for help if their scores don’t make sense or if the score doesn’t match their presentation of distress. If not, ask the client to redo the ORS. When all else fails, don’t argue with the client or enter invalid data. BON includes a feature that allows you to exclude an invalid rater (client) from your stats.





.png)


.png)